New Parents and a Newborn with Sickle Cell Disease: What Now?
By Dr. Kevin Williams, Chief Medical Officer for Rare Disease at Pfizer Published June 27, 2019

In this article, I’d like to introduce you to TaLana Hughes, a mother of three who is also the executive director of the Sickle Cell Disease Association of Illinois (SCDAI). TaLana has one child with SCD and two children with the sickle cell trait.
For the last two years, I’ve been honored to talk with you about sickle cell disease (SCD) through this column, sharing important information and my perspectives as a medical professional. Now, as the “Ask Dr. Kevin” series enters its third year, I wanted to change things a bit by letting you also hear directly from those who matter most—people living with SCD and their caregivers.
As TaLana knows from both personal experience and through her work with SCDAI, learning that your child has SCD can feel overwhelming and scary. While family and friends can be an important source of support, they may not always know the best way to help—and parents may find it hard to explain what they need.
In order to help people better understand what it’s like to be a parent of a newborn with SCD, and how family and friends can be most helpful, TaLana and I share our thoughts below on some of the most common questions we’ve been asked about the topic.
What are the biggest fears and challenges parents face upon learning their child has SCD?
TaLana: Immediately after my child received the diagnosis, my husband and I experienced an initial wave of shock and fear. It became suddenly apparent that both of us have the sickle cell trait which we passed down to our child. After the initial shock wore off, a million questions started to run through our minds, and we wondered what this would ultimately mean for our daughter.
Dr. Kevin: I know that for many parents, an SCD diagnosis can certainly be overwhelming, and I see how parents may fear the worst. However, it’s important to know that in recent years we’ve seen advances in understanding and scientific breakthroughs that are potentially paving the way for better care of people with SCD.
I also can’t stress enough to new parents the importance of setting up a healthcare team for their child as soon as possible. Receiving care early and often can help reduce the impacts and complications of the disease. SCD takes a toll on all systems of the body, so having a team made up of a pediatric hematologist, primary care doctor, and other specialists, such as an eye doctor, pulmonologist, cardiologist, and dentist, is key to the health of the child.
What are some tips for helping parents cope with the news?
TaLana: I know that I needed time to digest the news to really understand how the diagnosis would impact our child and family. Once I had a stronger understanding of the disease and how it would manifest over time as my child grew, I started to have a better idea of the support needed from my family and our local community.
Dr. Kevin: I’ve seen incredible connections and support systems form when parents of a child with SCD talk with other parents going through the same thing. There’s a certain comfort that comes from talking to those who have “been there, done that.” Parents can meet other families through local community groups, online platforms like oneSCDvoice*,which includes curated content and a wealth of information for those in the SCD community, and the Sickle Cell Disease Association of America (SCDAA), which publishes a calendar of local SCD events around the country.
How can family and friends offer support?
TaLana: I tell parents of children with SCD to educate their loved ones about the disease and to communicate how it affects your child. Teaching others about the condition gives me the opportunity to explain what kind of specific support I need. It also allows my family and friends to figure out how to best provide support—whether it be a ride to an appointment, a change of clothes for an overnight stay in the hospital, or help with small chores at home.
Dr. Kevin: I also encourage family members and friends to learn as much as they can on their own, because there are still a number of misperceptions about the disease. For example, the belief that a baby born with SCD will die before reaching adulthood. As I mentioned in a previous article, this is a myth! The majority of children with SCD live to adulthood, thanks to advances in SCD care. However, the life expectancy of someone with SCD in the US is only between 40 and 60 years, compared to average US life expectancy of 78.8 years. By understanding the truths about SCD, family and friends are in a better position to provide meaningful support and be allies.
What tools are most helpful for new parents caring for their child with SCD?
TaLana: I always carry a notebook with me so I can take notes and keep track of my child’s “baseline” and SCD history to see how the disease manifests over time. I have an overnight bag in my trunk that includes a change of clothes and snacks. I carry a thermometer in my purse to take my child’s temperature and an incentive spirometer to help facilitate stronger breathing. I’ve also joined a group chat with other parents who have children with SCD, and this has been one of my most important tools for connecting with and learning from other parents who share this experience.
Dr. Kevin: These are great suggestions. I would also encourage parents to connect with their local SCD organization, like an SCDAA local chapter. With a disease like SCD, which is rare in the US and often misunderstood, connecting with others who have similar experiences and challenges is so important for building your support system.
Do infants experience pain crises? What are the warning signs? What is your best advice for new parents when it comes to handling a newborn having a crisis?
TaLana: Yes, infants can have pain crises. However, because they can’t communicate with words and explain any pain they are experiencing, recognizing pain crises can be difficult. In my own experience, the first warning signs are usually dactylitis, where the hands and feet begin to swell, and a fever. However, because new parents usually pay attention to anything out of the ordinary seen in their newborn, they often are able to notice how their own child displays warning signs.
When it comes to noticing something out of the ordinary in my child, I always play it safe. I also find it really beneficial to speak with other parents with children who have SCD and to learn about what they see in their own children and discuss how they’ve handled episodes of pain.
Dr. Kevin: It’s also important for parents to understand that pain crises are unfortunately a universal experience for people with SCD. Crises typically manifest in infants aged six months and older, and they are often unpredictable and can occur up to several times a year. So, to TaLana’s point, learning to recognize what a pain crisis looks like in their child will help parents know when to seek help.
What do babysitters or other caregivers need to know?
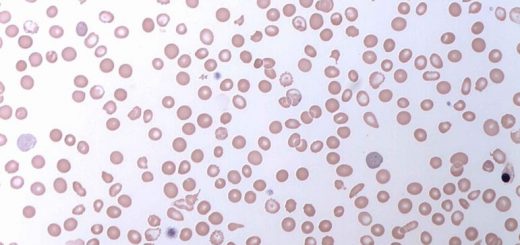
TaLana:I make sure other caregivers and babysitters know about my child’s personal regimens and what to do in case of an emergency. I share important pointers, like to make sure my child is hydrated and never around smoke, which can increase the risk of Acute Chest Syndrome (ACS), a bout of pneumonia or a serious lung condition due to the sickling of red blood cells, in people with SCD.
Lastly, I make sure they know how special my child is and all the wonderful qualities she has. I tell them her likes and dislikes, hobbies and interests, and what makes her laugh. Having SCD may be a normal part of my child’s life, but I make sure she is not defined by her condition.
Dr. Kevin: I agree wholeheartedly. Children with SCD are children first and foremost. While the disease affects them, it certainly does not define them—nor should SCD or any disease define the person who has it.
For more information about parenting a child with SCD, check out “A Parents Handbook for Sickle Cell Disease” and the CDC’s “5 Facts You Should Know about SCD.”
Keep up to date on Pfizer’s SCD efforts by visiting our page here. You can also follow Pfizer on Facebookand Twitter.
*Supported by Pfizer
The “Ask Dr. Kevin” series is brought to you by Pfizer Rare Disease in collaboration with the National Newspaper Publishers Association (NNPA) to increase understanding of sickle cell disease.
Dr. Kevin Williams is the Chief Medical Officer for Rare Disease at Pfizer where he leads a Medical Affairs organization of approximately 150 medical colleagues around the globe. He pursued medicine after being inspired by his father’s work as a general practitioner in his hometown of Baton Rouge, Louisiana. Dr. Kevin is passionate about raising awareness and increasing understanding of rare diseases, such as sickle cell disease, in the African American community.


Recent Comments