CIRM and NHLBI Collaborating to Fund Cell and Gene Therapies for Sickle Cell Disease

The California Institute for Regenerative Medicine (CIRM) and the National Heart, Lung and Blood Institute (NHLBI) have entered into a “landmark” collaboration to co-fund and help speed the development of cell and gene therapies to cure sickle cell disease (SCD), according to a press release.
The agreement was created under the National Institutes of Health’s “Cure Sickle Cell” initiative, led by NHLBI, the goal of which is to take advantage of the latest genetic discoveries and technological advances to move the most promising genetic-based therapies into clinical trials within five to 10 years.
This new collaboration will take advantage of CIRM’s vast resources and expertise, which have already resulted in more than 50 clinical trials in stem cell and regenerative medicine, and will provide lines of co-funding to CIRM-sponsored research.
“There is a real need for a new approach to treating SCD and making life easier for people with SCD and their families,” said Adrienne Shapiro, mother of a child with the disease and co-founder of Axis Advocacy.
“Finding a cure for Sickle Cell would mean that people like my daughter would no longer have to live their life in short spurts, constantly having their hopes and dreams derailed by ER visits and hospital stays. It would mean they get a chance to live a long life, a healthy life, a normal life.”
One of the eligible projects is a gene therapy approach to cure SCD headed by Mark Walters, MD, a pediatric hematologist and oncologist at UCSF Benioff Children’s Hospital in Oakland, California.
CIRM granted $4.46 million to Walters in April to pursue a therapeutic translational project to develop a cure based on the autologous transplant of CRISPR/Cas9 gene-edited stem cells. An autologous transplant requires a patient’s own stem cells, rather than a donor’s, bypassing donor requirements and eliminating the risks of graft-versus-host disease and rejection.
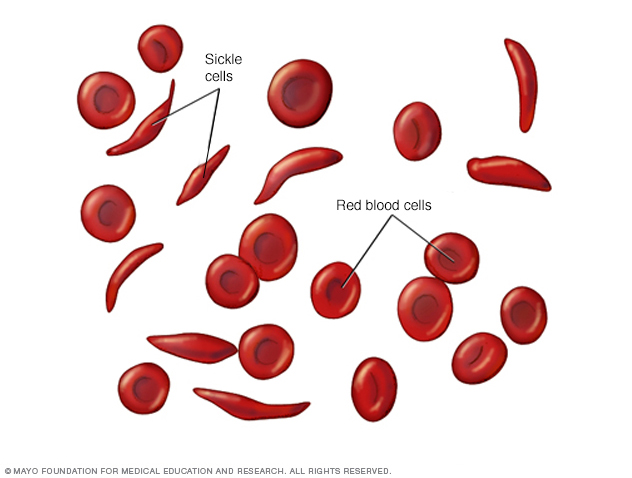
Walters and his team plan to collect patients’ own hematopoietic (blood-forming) stem cells (HSCs) from the bone marrow, into laboratory cultures, where they will be genetically edited by CRISPR-Cas9 to correct the HBB mutation underlying sickle cell disease. The corrected HSCs will then be introduced back into the patient to produce new, healthy red blood cells. According to the project description, this approach could make a cure universally available because it corrects the sickle mutation in a person’s own stem cells.
For now, the main goal is to establish the optimal protocol for gene editing and stem cell production, laying the groundwork to get approval from the U.S. Food and Drug Administration for trials in patients.
So far, CIRM has granted more than $38 million to several different preclinical and clinical-stage projects targeting SCD.
Two other cell and gene therapy approaches funded by the agency are already being explored in a Phase 1 trial (NCT03249831) at City of Hope Medical Center and a Phase 1/2 trial (NCT02247843) at University of California Los Angeles. Both trials are still recruiting participants.
“CIRM currently has 23 clinical stage programs in cell and gene therapy. Given the advancements in these approaches for a variety of unmet medical needs, we are excited about the prospect of leveraging this to NIH-NHLBI’s Cure Sickle Cell Initiative,” said Maria T. Millan, MD, president and CEO of CIRM. “We are pleased the NHLBI sees value in CIRM’s acceleration and funding program and look forward to the partnership to accelerate cures for sickle cell disease.”


Recent Comments